Pancreatitis: A Simple Guide to Symptoms, Causes, and Treatment

Severe abdominal pain can be a significant cause for concern. When it appears suddenly, it is often difficult to know the cause or what to do next. This type of pain is one of the most common signs of pancreatitis, a condition caused by inflammation of the pancreas. Navigating complex medical terminology and understanding the difference between a short-term issue and a long-term condition can be a major challenge.
This guide provides a clear, straightforward explanation of pancreatitis. We will help you recognise the key symptoms of its acute and chronic forms. You will learn about the main causes and risk factors associated with the condition. Finally, we will outline how pancreatitis is treated and managed in the UK, giving you the essential information you need to understand its potential impact on daily life and independence.
Understanding Pancreatitis: What It Is and Why It Happens
Pancreatitis is the medical term for inflammation of the pancreas, a vital gland located behind the stomach. The condition occurs when digestive enzymes, which should only become active in the small intestine, activate prematurely while still inside the pancreas. This early activation causes the enzymes to irritate the pancreas itself, leading to swelling, inflammation, and damage to its tissues.
To better understand this concept, watch this helpful video:
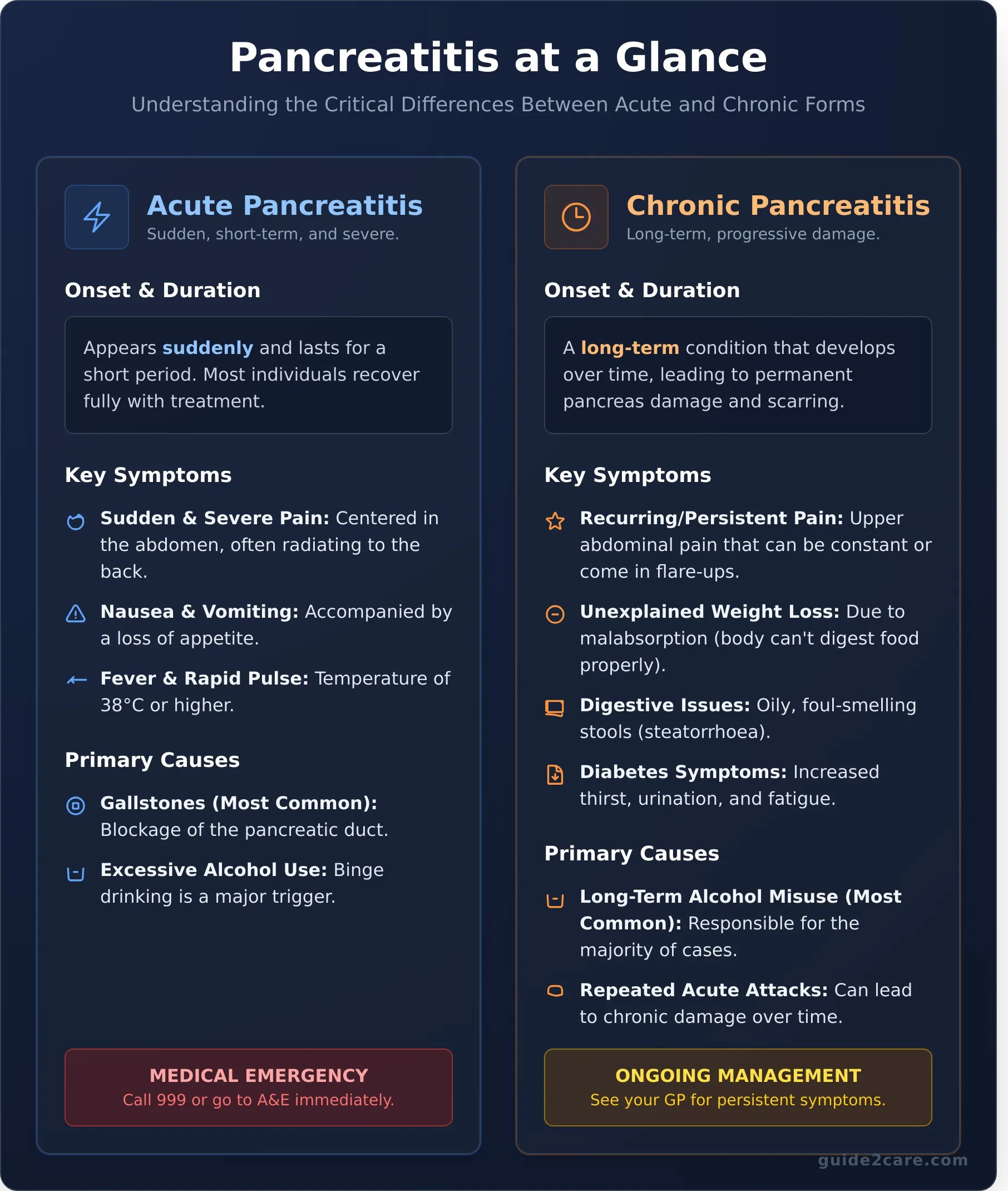
Acute vs. Chronic Pancreatitis: The Key Differences
There are two primary forms of the condition. Acute pancreatitis appears suddenly and typically lasts for a short period. While it can be a severe medical event requiring hospitalisation, most individuals recover fully with appropriate treatment. In contrast, chronic pancreatitis is a long-term, persistent condition where inflammation does not heal, leading to permanent scarring and damage to the organ over time. Repeated episodes of acute pancreatitis can eventually result in the chronic form.
The Role of the Pancreas in Your Body
The pancreas performs two essential jobs, and inflammation disrupts its ability to carry them out effectively. For a comprehensive overview of pancreatitis and its impact, it is useful to understand these core roles:
- Aiding Digestion: The pancreas produces powerful enzymes that travel to the small intestine to break down fats, proteins, and carbohydrates from food. When the pancreas is inflamed, it may not produce or release enough enzymes, leading to problems with digestion and nutrient absorption.
- Regulating Blood Sugar: It creates crucial hormones, including insulin and glucagon, which are released directly into the bloodstream. These hormones work together to control the body's blood sugar (glucose) levels. Damage from pancreatitis can impair hormone production, sometimes leading to diabetes.
Recognising the Symptoms of Pancreatitis
Identifying the signs of pancreatitis is crucial for seeking timely medical care. The symptoms vary significantly depending on whether the condition is acute (sudden and short-term) or chronic (long-lasting). Because some signs can be mistaken for other digestive problems, it is important to understand the key indicators. Sudden and severe abdominal pain should never be ignored and always requires immediate medical attention.
Symptoms of Acute Pancreatitis
Acute pancreatitis develops quickly and its primary symptom is intense pain. The signs often appear without warning and can be severe. Key symptoms include:
- A sudden, severe, and persistent pain in the centre of your abdomen.
- Pain that radiates from your abdomen to your back.
- Feeling or being sick (nausea and vomiting) and a loss of appetite.
- A high temperature (fever) of 38C or above and a rapid pulse.
- Tenderness or swelling of the abdomen.
Symptoms of Chronic Pancreatitis
Chronic pancreatitis is a long-term condition where the pancreas becomes permanently damaged. Its symptoms can be persistent or occur in flare-ups. Understanding these long-term symptoms is the first step in getting a correct diagnosis. The U.S. National Institute of Diabetes and Digestive and Kidney Diseases provides detailed information on how pancreatitis is diagnosed and treated, which can help you prepare for conversations with your doctor. Common signs include:
- Recurring or persistent upper abdominal pain, which can be severe.
- Unexplained weight loss, as your body cannot digest food properly (malabsorption).
- Oily, foul-smelling stools that are difficult to flush (steatorrhoea).
- Symptoms of diabetes, such as feeling very thirsty, needing to urinate frequently, and fatigue.
When to Seek Urgent Medical Help
It is vital to know when to get medical assistance for abdominal pain. Follow these clear guidelines to ensure you receive the right care at the right time.
- Call 999 or go to A&E immediately if you experience sudden, severe pain in your abdomen. This is a medical emergency.
- See your GP if you have persistent or recurring symptoms that are causing you concern, such as ongoing abdominal pain, unexplained weight loss, or changes in your stools.
- Contact NHS 111 if you need urgent medical advice but it is not a life-threatening situation.
Common Causes and Key Risk Factors
Understanding the causes of pancreatitis is the first step toward prevention and management. In the UK, the condition is most often triggered by two primary factors: gallstones and excessive alcohol consumption. However, in a significant number of cases, a specific cause cannot be identified. This is known as idiopathic pancreatitis.
Most risk factors are linked to lifestyle, which means modifications can often reduce your risk of developing the condition.
The Main Causes of Acute Pancreatitis
Acute pancreatitis occurs suddenly and is typically caused by a specific trigger. The most common causes include:
- Gallstones: These small, hard deposits can travel out of the gallbladder and block the opening of the pancreatic duct. This blockage traps digestive fluids inside the pancreas, leading to inflammation and pain.
- Excessive Alcohol Consumption: Binge drinking or heavy alcohol use is a major trigger for acute attacks. The exact process is complex, but alcohol is directly toxic to pancreatic cells.
Less common triggers for an acute attack can include an injury to the abdomen, certain medications, or complications from a medical procedure.
Factors Leading to Chronic Pancreatitis
Chronic pancreatitis develops over time and involves permanent damage to the pancreas. The leading causes are:
- Long-term Alcohol Misuse: This is the most significant factor, responsible for the majority of chronic cases in the UK.
- Repeated Acute Attacks: Each episode of acute pancreatitis can cause scarring. Over time, this cumulative damage can lead to chronic disease and a loss of pancreatic function.
- Other Conditions: Autoimmune diseases, where the body’s immune system attacks the pancreas, and certain genetic or hereditary factors can also lead to the chronic form of the condition.
Other Potential Risk Factors
Several other factors can increase your likelihood of developing pancreatitis. Understanding the full range of symptoms and risk factors of pancreatitis is crucial for early detection and prevention. Key risk factors include:
- Smoking tobacco
- Obesity
- A family history of the condition
- High levels of calcium in the blood (hypercalcaemia)
- Very high levels of fats (triglycerides) in the blood
How Pancreatitis Is Diagnosed and Treated
A doctor will diagnose pancreatitis based on your symptoms, a physical examination, and your medical history. To confirm the condition, a series of tests are required. Treatment aims to manage symptoms and support the body, allowing the pancreas time to recover. For acute cases, this almost always requires a stay in hospital.
Confirming a Diagnosis
To confirm a diagnosis and determine the severity of the inflammation, your doctor will arrange for specific tests. These provide a clear picture of what is happening to the pancreas and surrounding organs.
- Blood tests: These are used to measure the levels of two digestive enzymes, amylase and lipase. High levels are a key indicator of acute pancreatitis.
- Imaging tests: A CT scan, MRI, or abdominal ultrasound creates images of your pancreas. These scans can show inflammation, fluid collections, or identify a cause like gallstones.
- Stool tests: In cases of suspected chronic pancreatitis, a stool sample may be analysed to check how effectively your body is absorbing fats from food.
Treatment for Acute Pancreatitis
Treatment for an acute attack takes place in hospital, where your condition can be closely monitored. The focus is on supporting your body while the inflammation subsides.
- Intravenous (IV) fluids: You will receive fluids directly into a vein to prevent dehydration.
- Pain relief: Pancreatitis can be very painful, so effective pain relief medication is a priority.
- Nutritional support: You may be advised to stop eating for a few days to allow your pancreas to rest. Food is then gradually reintroduced, starting with clear fluids and low-fat foods.
Managing Chronic Pancreatitis Long-Term
Managing the long-term effects of chronic pancreatitis involves significant lifestyle adjustments and ongoing medical support to control symptoms and prevent further damage.
- Lifestyle changes: It is essential to stop drinking alcohol and to quit smoking entirely, as both can worsen the condition.
- Pain management: Controlling chronic pain can be challenging and may require a referral to a specialist pain management clinic.
- Pancreatic enzyme supplements (PERT): If the pancreas can no longer produce enough digestive enzymes, you will be prescribed PERT capsules to take with meals to aid digestion.
- Dietary management: A dietitian will provide guidance on a suitable low-fat diet to reduce symptoms and ensure you get enough nutrients.
Living with Pancreatitis: Diet, Lifestyle, and Care Support
Managing pancreatitis long-term requires careful attention to diet, lifestyle, and ongoing medical supervision. Making practical changes to your daily routine is essential to reduce symptoms, prevent flare-ups, and protect the pancreas from further damage.
Key Dietary and Lifestyle Adjustments
The primary goal of lifestyle changes is to reduce the strain on your pancreas. Adhering to medical advice is crucial for managing the condition effectively. Key adjustments include:
- A strict low-fat diet: High-fat foods stimulate the pancreas to release digestive enzymes, which can trigger pain. Focus on lean proteins, fruits, vegetables, and whole grains.
- Smaller, more frequent meals: Eating six small meals throughout the day is often easier for the pancreas to manage than three large ones.
- Complete abstinence from alcohol and smoking: Alcohol is a primary cause of pancreatitis and must be avoided entirely. Smoking can accelerate damage and increase complication risks.
- Staying well-hydrated: Drinking plenty of water supports digestion and overall health. Dehydration can worsen symptoms.
Long-Term Complications and Monitoring
Chronic pancreatitis can lead to other serious health issues over time. Damage to the pancreas may impair its ability to produce insulin, significantly increasing the risk of developing diabetes. Malnutrition and vitamin deficiencies are also common, as the body may struggle to absorb fats and essential nutrients from food. Because of these risks, regular follow-up appointments with a GP or specialist are vital. These check-ups allow for proactive monitoring of your condition and early management of any complications.
When Pancreatitis May Require Extra Support
The persistent symptoms of pancreatitis can sometimes make daily living a challenge. Chronic pain can limit mobility and the ability to perform everyday tasks, while complex dietary needs can make meal preparation difficult. In these situations, additional support may become necessary. Domiciliary care, or care at home, can provide practical help with medication management, personal care, and preparing suitable meals. If managing daily tasks becomes difficult, professional support can make a significant difference. Explore care options in your area to find the help you need.
Key Steps for Managing Pancreatitis
Understanding the fundamentals of pancreatitis is the first step toward effective management. The key takeaways are clear: recognise the distinct symptoms for prompt action, strictly follow the treatment plan prescribed by your GP or specialist, and commit to essential lifestyle adjustments, particularly concerning diet and alcohol intake. These actions form the foundation for controlling the condition and improving your quality of life.
For many, managing a long-term health condition requires practical support at home. Whether you need assistance with daily tasks, specialised meal planning, or more complex domiciliary care, finding the right provider is essential. The process of searching for and vetting care services can be complex, but resources are available to simplify it.
Guide2Care provides a straightforward directory of care providers across the UK. Use our resources to locate the specific support you require to manage your health effectively. Find the care you need with the Guide2Care directory.
Frequently Asked Questions
Can pancreatitis be completely cured?
Acute pancreatitis can often be resolved if the underlying cause, such as gallstones, is treated. In these instances, the pancreas may return to normal function. However, chronic pancreatitis is a long-term condition that cannot be cured. Management focuses on controlling symptoms, preventing further damage to the pancreas, and managing complications. Consistent medical care and lifestyle adjustments are essential for managing the chronic form of the condition.
Is pancreatitis a hereditary condition?
While most cases are linked to factors like gallstones or alcohol consumption, a hereditary form does exist. Certain genetic mutations can significantly increase a person's risk of developing the condition, often from a young age. If multiple family members have experienced pancreatitis, genetic testing may be recommended by a specialist. For the majority of patients, the condition is not directly inherited but caused by other health and lifestyle factors.
What is a typical pancreatitis-friendly diet?
A pancreatitis-friendly diet is low in fat and high in nutrients. Focus on lean proteins like skinless chicken and fish, whole grains, fruits, and vegetables. It is crucial to avoid high-fat foods, including fried items, full-fat dairy, red meat, and processed snacks. Small, frequent meals are often better tolerated than three large ones. Abstaining from alcohol completely is a critical part of the dietary plan to allow the pancreas to heal and prevent flare-ups.
Can stress cause or worsen pancreatitis?
Stress is not considered a direct cause of pancreatitis. However, it can significantly worsen the condition, especially for those with the chronic form. High stress levels can trigger flare-ups and intensify symptoms like pain. Furthermore, stress may lead to unhealthy coping mechanisms, such as poor dietary choices or alcohol use, which are known risk factors. Managing stress is therefore an important part of a comprehensive care plan for pancreatitis.
How does chronic pancreatitis affect life expectancy?
Chronic pancreatitis can reduce life expectancy, but the impact varies depending on several factors. Continued alcohol consumption and smoking are the most significant contributors to a poorer prognosis. The development of complications, such as diabetes or pancreatic cancer, also affects life expectancy. With diligent medical management, complete abstinence from alcohol and tobacco, and a healthy lifestyle, many individuals can manage the condition effectively and improve their long-term outlook.