What is Fibromyalgia? A Simple Overview of Symptoms and Management

Widespread pain, persistent fatigue, and difficulty concentrating can make daily life a challenge. When these symptoms have no obvious cause, it is often difficult to get a clear diagnosis or feel understood. These experiences are common for those living with fibromyalgia, a long-term condition that affects how the body processes pain signals and can significantly impact your wellbeing.
Given the condition's connection to the central nervous system, some individuals also explore complementary therapies focused on spinal alignment. For those interested in this path, the online directory Upper Cervical Care can help connect them with specialized practitioners.
This guide provides a straightforward overview of fibromyalgia. We explain the condition in simple terms, breaking down complex medical information into clear, manageable sections. You will learn about the common symptoms, how the condition is diagnosed within the UK, and discover practical steps you can take to manage your daily activities. We also outline the support systems available to help you maintain your independence and find the care you need.
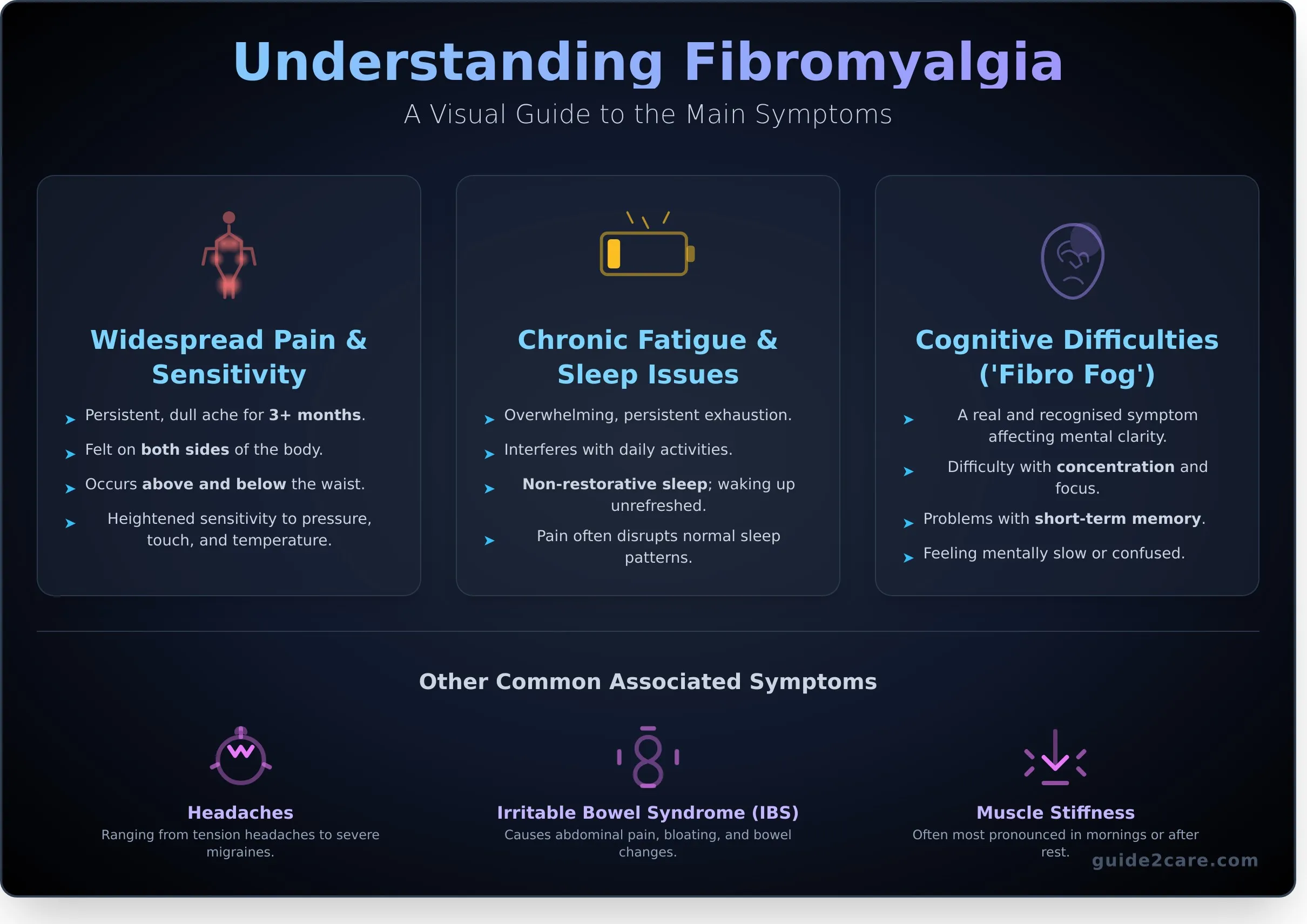
Understanding the Main Symptoms of Fibromyalgia
Fibromyalgia is a long-term condition that presents a unique combination of symptoms which can vary significantly between individuals. While a comprehensive overview of fibromyalgia details its complexity, its three core symptoms are widespread pain, persistent fatigue, and cognitive difficulties. Recognising these is the first step toward seeking a diagnosis and managing the condition. Symptoms can also fluctuate in severity; periods of increased intensity are often called 'flares'.
Widespread Pain and Increased Sensitivity
The primary symptom is a persistent, dull, aching pain that is felt on both sides of the body, both above and below the waist. For a diagnosis, this pain must have been present for at least three months. Many people also experience a heightened sensitivity to stimuli that are not normally painful. This can include sensitivity to pressure, touch, temperature changes, and even bright lights or loud noises.
Chronic Fatigue and Sleep Problems
The fatigue associated with this condition is not simple tiredness. It is an overwhelming and persistent exhaustion that can interfere with daily activities. Despite sleeping for long periods, individuals often wake up feeling unrefreshed. This non-restorative sleep is common, as widespread pain can disrupt normal sleep patterns and may be linked to other sleep disorders.
Cognitive Difficulties ('Fibro Fog')
Many people experience cognitive issues, commonly referred to as 'fibro fog'. This is a real and recognised symptom that affects mental clarity. It can manifest as difficulty concentrating, problems with short-term memory, and a general feeling of being mentally slow or confused. These challenges can make completing mental tasks at work or home more difficult.
Other Common Associated Symptoms
In addition to the main symptoms, other conditions are often present. It is important to be aware of these as they can also impact quality of life. Common associated symptoms include:
- Headaches, ranging from tension headaches to severe migraines.
- Irritable bowel syndrome (IBS), causing abdominal pain, bloating, and changes in bowel habits.
- Muscle stiffness, which is often most pronounced in the mornings or after periods of rest.
What Causes Fibromyalgia and Who is at Risk?
The exact cause of fibromyalgia is not yet known. However, research points towards a problem with how the central nervous system (the brain, spinal cord, and nerves) processes pain signals throughout the body. This leads to the widespread pain and fatigue characteristic of the condition. It is important to understand that fibromyalgia is not a degenerative, autoimmune, or inflammatory disease, meaning it does not cause damage to muscles or joints.
The Role of the Central Nervous System
The leading theory behind fibromyalgia is a phenomenon called 'central sensitisation'. In simple terms, this means the central nervous system becomes highly sensitive to pain. You can think of it as the brain’s 'volume knob' for pain signals being permanently turned up too high.
This heightened sensitivity causes the brain and nerves to overreact to both painful and non-painful stimuli. A light touch that would not normally hurt might be felt as painful. This process is thought to be influenced by an imbalance of certain brain chemicals (neurotransmitters) that regulate mood and pain, such as serotonin and noradrenaline. Lower levels of these chemicals can affect how the body deals with pain.
Potential Triggers and Risk Factors
In some people, the symptoms of fibromyalgia develop gradually with no single identifiable cause. For others, the condition appears to be triggered by a specific event. There are also several known risk factors that make an individual more likely to develop the condition. Understanding these is a key part of the diagnostic process; for official guidance, the NHS provides comprehensive information on Fibromyalgia diagnosis and treatment in the UK.
Key risk factors and potential triggers include:
- Stressful Events: A physically or emotionally traumatic event, such as a car accident, a serious infection, childbirth, or the death of a loved one, can sometimes precede the onset of symptoms.
- Gender: The condition affects significantly more women than men. The reasons for this are not fully understood but may involve hormonal factors.
- Genetics: The condition often runs in families. If you have a close relative with fibromyalgia, your own risk of developing it is higher, which suggests a genetic predisposition.
- Existing Rheumatic Conditions: People with other conditions like osteoarthritis, rheumatoid arthritis, or lupus are more likely to also be diagnosed with fibromyalgia.
How Fibromyalgia is Diagnosed in the UK
Diagnosing fibromyalgia is a process of careful assessment and elimination, as there is no single, definitive test like a blood test or scan. A doctor makes a diagnosis based on a patient's symptoms, a physical examination, and by ruling out other conditions that cause similar issues. The entire diagnostic process begins with a visit to your GP.
Visiting Your GP: The First Step
To get the most from your appointment, it is helpful to prepare. Keep a diary for a few weeks to track your symptoms. Note where you feel pain, its severity, and what makes it better or worse. Also, record your fatigue levels, sleep quality, and any memory or concentration problems. Your GP will ask about these symptoms and will conduct a physical examination, which may involve gently pressing on certain areas of your body to assess your pain.
The Diagnostic Criteria
Doctors use established criteria to identify fibromyalgia. The primary requirement is widespread pain that affects both sides of the body, as well as areas both above and below the waist. For a diagnosis to be considered, these symptoms must have been consistently present for at least three months. The doctor will also evaluate the severity of other key symptoms, such as persistent fatigue, waking up feeling unrefreshed, and cognitive difficulties (often called 'fibro fog').
Ruling Out Other Conditions
Because the symptoms of fibromyalgia overlap with many other health problems, your GP will likely order blood tests. It is important to understand that these tests are not to find fibromyalgia, but to exclude other conditions. When test results come back normal, it helps to confirm that another illness is not the cause of your symptoms.
Conditions with similar symptoms include:
- Rheumatoid arthritis
- An underactive thyroid (hypothyroidism)
- Multiple sclerosis (MS)
- Chronic fatigue syndrome (ME/CFS)
If these other conditions are ruled out and your symptoms align with the recognised criteria, your GP can make a confident diagnosis.
Managing Fibromyalgia: Treatments and Lifestyle Changes
While there is currently no cure for fibromyalgia, a combination of treatments can effectively manage symptoms. The primary goal is to reduce pain and improve your overall quality of life. Finding the right approach is a personal process, often involving trial and error. A multi-faceted plan that includes medical support, physical activity, and self-care strategies typically yields the best results.
Medical Treatments Available on the NHS
Your GP will work with you to create a suitable treatment plan. This may include prescribing certain antidepressant medications, which can help to reduce pain and fatigue. It is important to note that common painkillers are often not effective for the type of pain caused by this condition. You may also be referred for talking therapies, such as Cognitive Behavioural Therapy (CBT), to help you develop practical coping strategies.
The Importance of Movement and Gentle Exercise
Regular, gentle exercise is one of the most effective ways to manage symptoms. It is vital to start slowly and build up your activity level over time. Activities like walking, swimming, cycling, and yoga can help to increase your stamina and flexibility while reducing stiffness and pain. The key is consistency and listening to your body to avoid overexertion.
Lifestyle Adjustments for Daily Living
Making small changes to your daily routine can have a significant impact on managing your condition. Consider implementing the following strategies:
- Pacing: Learn to balance periods of activity with rest. This helps you conserve energy and can prevent symptom flare-ups.
- Improving Sleep: Establish a regular sleep schedule and create a relaxing bedtime routine. Ensure your bedroom is dark, quiet, and at a comfortable temperature.
- Stress Management: Find techniques that help you relax. Many people find mindfulness, meditation, or deep-breathing exercises beneficial for reducing stress levels, which can otherwise worsen symptoms.
Living with Fibromyalgia: Support and Long-Term Care
Managing a long-term condition like fibromyalgia requires a practical approach to support. The fluctuating nature of symptoms like chronic pain and severe fatigue can make everyday life unpredictable. Building a reliable support network and knowing when to ask for help are essential for maintaining your well-being and independence. A range of UK resources, charities, and formal care options are available to provide assistance.
Finding UK Support Groups and Charities
Connecting with others who have similar experiences can significantly reduce feelings of isolation. National charities are a primary source of reliable information and community support. Key UK organisations include:
- Fibromyalgia Action UK: A national charity offering a helpline, benefit support, and information packs.
- Versus Arthritis: Provides comprehensive resources on managing pain and living with related long-term conditions.
These groups facilitate local meetings and online forums, allowing you to share coping strategies and receive valuable peer support.
When Daily Tasks Become Difficult
The physical and cognitive symptoms of the condition can impact your ability to complete routine tasks. Activities like cooking, cleaning, and shopping can become draining. It is important to learn energy conservation techniques, such as pacing yourself and breaking large tasks into smaller steps. Simple home adaptations, like placing a stool in the kitchen, can also help. Seeking help is a proactive strategy for managing symptoms and preserving energy for the things you enjoy.
Exploring Care Options for Support at Home
When daily tasks become consistently overwhelming, home care (also called domiciliary care) offers a practical solution. This support is flexible and tailored to your specific needs. A professional carer can visit your home to assist with a range of duties, from personal care and meal preparation to housework and attending appointments. By delegating physically demanding chores, you can better manage your energy levels and prevent symptom flare-ups. Support can be arranged for a few hours a week or for more comprehensive daily assistance. Find local home care providers to help manage daily life.
Managing Fibromyalgia: Key Takeaways and Next Steps
Understanding and managing fibromyalgia is a journey, but it is one that can be navigated successfully with the right approach. This complex condition is defined by widespread pain, fatigue, and cognitive difficulties, but a clear diagnosis is the first step toward control. In the UK, management focuses on a personalised combination of treatments, including medication, therapy, and crucial lifestyle changes like gentle exercise and stress reduction. Creating a sustainable plan is key to improving your long-term well-being.
Building a robust support network is essential for living well with a chronic condition. For those who require practical assistance with daily tasks to conserve energy and manage symptoms effectively, professional domiciliary care can be an invaluable resource. If you are exploring your options, our platform simplifies the process. Use our directory to find rated home care agencies near you.
With the right information, a proactive care plan, and the proper support, it is possible to lead a full and active life. Taking informed steps today empowers you for a better tomorrow.
Frequently Asked Questions About Fibromyalgia
Is fibromyalgia a real illness?
Yes, fibromyalgia is a real medical condition recognised by the NHS and the World Health Organisation. It is a long-term (chronic) condition characterised by widespread pain, profound fatigue, and cognitive disturbances, often called "fibro fog." Diagnosis is typically made based on a patient's symptoms and by ruling out other conditions, as there is no single definitive test for the illness.
Can fibromyalgia go away or does it get worse over time?
Fibromyalgia is a chronic condition, meaning it is long-term and currently has no cure. However, it is not considered a progressive illness and does not necessarily worsen over time. Symptoms often fluctuate, leading to periods of increased severity known as flare-ups, as well as periods of remission. Consistent management through treatment and lifestyle changes can help control symptoms and improve daily function.
Does a specific diet help with fibromyalgia symptoms?
There is no single diet officially recommended for fibromyalgia. However, many individuals find that a balanced diet rich in fruits, vegetables, and lean protein helps manage their energy levels and overall wellbeing. Some people identify specific food triggers, such as caffeine, artificial sweeteners, or gluten, that worsen their symptoms. Keeping a food diary is a practical way to track your diet and identify potential sensitivities.
Is fibromyalgia considered a disability in the UK?
In the UK, fibromyalgia can be classified as a disability under the Equality Act 2010. This applies if the condition has a substantial and long-term adverse effect on your ability to perform normal day-to-day activities. An individual may be eligible for support such as workplace adjustments or benefits like Personal Independence Payment (PIP), but eligibility is determined by a thorough assessment of how the condition affects you.
What activities or foods should be avoided with fibromyalgia?
To manage fibromyalgia, it is often advised to avoid overexertion, which can lead to a "boom and bust" cycle of activity followed by a severe flare-up. Pacing is a key strategy. While food triggers are individual, common ones to consider avoiding include excessive caffeine, monosodium glutamate (MSG), aspartame, and highly processed foods. Identifying personal triggers often requires a process of careful observation and elimination.
How can I explain fibromyalgia to my family and friends?
Explain that fibromyalgia is an invisible illness with symptoms that can vary significantly from day to day. Use simple analogies, such as comparing the fatigue to having the flu or the pain to a constant, widespread toothache. Emphasise that your energy levels are unpredictable. You can also direct them to reliable resources, such as the NHS website or charities like Fibromyalgia Action UK, for further information.