Vascular Dementia: A Practical Guide for Families

Receiving a diagnosis can be an overwhelming experience, filled with complex medical terms and uncertainty about the future. For many families, understanding the specifics of vascular dementia and how it differs from other conditions like Alzheimer's disease is the first major hurdle. You may be asking what to expect as the condition progresses and what kind of support is required. This guide is designed to provide clear, practical answers to these critical questions.
We will walk you through the key symptoms to watch for, the typical stages of the condition, and the diagnostic process in the UK. You will gain a simple, clear understanding of available treatments and learn how to plan for future care needs, from domiciliary support to residential options. Our goal is to provide a reliable roadmap, equipping you with the information you need to make confident decisions and find the right support for your loved one.
What is Vascular Dementia? A Plain English Explanation
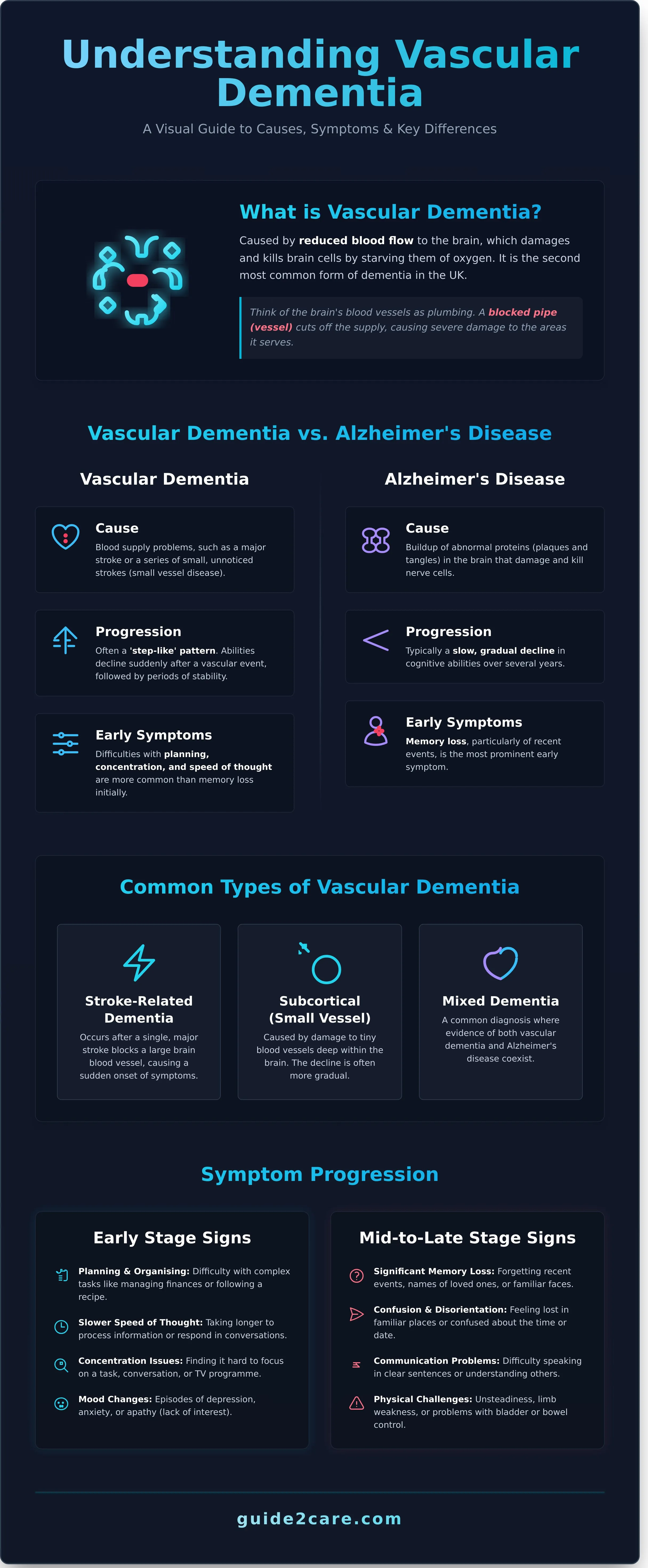
Vascular dementia is a condition caused by reduced blood flow to the brain, which damages and eventually kills brain cells. Think of the brain's blood vessels as the plumbing in a house. If a pipe gets blocked, the water supply to a room is cut off, causing damage. Similarly, when blood vessels in the brain are damaged, brain cells are starved of essential oxygen. This condition is the second most common type of dementia in the UK. For a detailed clinical overview, you can explore the question: What is vascular dementia?
This short video provides a clear visual explanation of how this happens.
The symptoms are different from the mild memory loss sometimes associated with normal ageing. The condition is directly linked to problems with the body's vascular system, which includes the heart and blood vessels. It often develops after a significant event like a stroke or as a result of a series of smaller, often unnoticed, strokes that cause cumulative damage over time.
How Vascular Dementia Differs from Alzheimer's Disease
While both are forms of dementia, their causes and progression differ. Alzheimer's disease is caused by the build-up of abnormal proteins in the brain. In contrast, vascular dementia results from blood supply problems. This difference often leads to a distinct pattern of decline. Instead of the slow, gradual progression seen in Alzheimer's, it can have a 'step-like' pattern, where abilities decline suddenly after a stroke and then remain stable. Early symptoms may also focus more on difficulties with planning and concentration rather than the memory loss typical of early Alzheimer's.
Common Types of Vascular Dementia
There are several main types, often categorised by their underlying cause.
- Stroke-related dementia: This can occur after a single, major stroke blocks a large blood vessel in the brain, causing a sudden onset of symptoms.
- Subcortical vascular dementia: Also known as small vessel disease, this type is caused by damage to the tiny blood vessels deep within the brain. The decline is often more gradual.
- Mixed dementia: A common diagnosis where an individual shows evidence of both vascular dementia and Alzheimer's disease. The two conditions coexist and contribute to the symptoms.
Recognising the Symptoms: Early and Later Stage Signs
The signs of vascular dementia can differ significantly from person to person. This is because symptoms depend on the specific area of the brain affected by reduced blood flow. Unlike the gradual decline often seen in other types of dementia, this condition frequently progresses in a 'step-like' pattern. A person may experience a sudden worsening of symptoms after a small stroke, followed by a period of stability.
For families, noting when these changes began and how they have progressed is crucial information for a GP. A clear timeline can assist with diagnosis and future care planning.
Early Stage Symptoms to Watch For
In the early stages, symptoms can be subtle and may be mistaken for normal signs of ageing. It is important to look for a consistent pattern of new or worsening difficulties. Common early signs include:
- Problems with planning and organising: Difficulty managing finances, following a sequence of tasks like cooking a meal, or making complex decisions.
- Slower speed of thought: Taking longer to process information or respond in conversations.
- Concentration issues: Finding it hard to focus on a task, a television programme, or a conversation for an extended period.
- Mild memory and language difficulties: Trouble finding the right word is common, though long-term memory may remain intact.
- Mood changes: Episodes of depression, anxiety, or apathy (a lack of interest in activities once enjoyed).
Symptoms in the Mid-to-Late Stages
As the condition progresses, the symptoms become more pronounced and begin to interfere more significantly with daily life. These changes often require more support from family or professional carers.
- Significant memory loss: Forgetting recent events, names of family members, or familiar faces.
- Increased confusion and disorientation: Feeling lost in familiar places or being confused about the time of day or date.
- Communication problems: Difficulty speaking in clear sentences or understanding what others are saying. A comprehensive guide to Recognising vascular dementia symptoms can provide further detail on these cognitive changes.
- Physical challenges: Unsteadiness on feet, limb weakness (often on one side of the body), or developing problems with bladder or bowel control.
- Behavioural changes: Increased agitation, aggression, restlessness, or wandering.
The Path to Diagnosis: What to Expect from the GP and Specialists
If you are concerned about memory loss or other cognitive symptoms for yourself or a loved one, the first step is to see a GP. A formal diagnosis is essential. It provides access to the right support, helps in planning for the future, and ensures any available treatments can be started. The GP will conduct an initial assessment and, if necessary, refer you to a specialist service for a more detailed evaluation.
The GP's goal is to understand the full picture of the person's health. They will listen to your concerns and may then refer to a UK specialist service, such as a memory clinic or a neurologist. These services are staffed by experts in diagnosing and managing conditions like vascular dementia.
Preparing for the Doctor's Appointment
To make the initial consultation as effective as possible, prepare in advance. It is helpful to bring clear information to the appointment. Consider accompanying your loved one to provide support and help recall details.
- List of symptoms: Note what the symptoms are, when they started, and how they affect daily life. For example, difficulty managing finances or forgetting recent events.
- Existing health conditions: Detail any other medical conditions, particularly a history of stroke, high blood pressure, diabetes, or heart problems.
- Current medications: Prepare a complete list of all prescribed drugs, over-the-counter medicines, and supplements.
Common Diagnostic Tests and Assessments
A diagnosis is rarely made from a single test. A specialist will use several methods to build a clear picture and rule out other conditions with similar symptoms.
- Cognitive tests: These are not exams to be passed or failed. They are a series of questions and tasks designed to assess memory, language skills, and problem-solving abilities.
- Brain scans: A CT or MRI scan can identify changes in the brain. For vascular dementia, doctors look for evidence of strokes or damage to the small blood vessels.
- Physical checks and blood tests: A physical examination, along with blood and urine tests, helps to exclude other causes of the symptoms, such as thyroid problems or vitamin deficiencies. Once a diagnosis is made, you can learn more about the NHS guidance on Treatments and support for vascular dementia to manage the condition effectively.
Managing Vascular Dementia: Treatments and Support Strategies
While there is currently no cure for vascular dementia, treatment can help slow its progression and manage symptoms. The primary goal is to address the underlying cardiovascular problems that cause the condition. A GP typically coordinates care with a multidisciplinary team, which may include neurologists, therapists, and dietitians, to create a personalised management plan.
Medical Treatments to Slow Progression
Medical intervention focuses on managing risk factors to prevent further damage to the brain. This is achieved by controlling conditions that affect blood vessel health. Common treatments include:
- Medication to manage high blood pressure (antihypertensives).
- Statins to lower high cholesterol.
- Drugs to manage diabetes and maintain stable blood sugar levels.
- Low-dose aspirin or other medications to reduce the risk of blood clots and further strokes, if prescribed by a doctor.
It is important to note that medications used for Alzheimer's disease are not typically effective for vascular dementia, unless a diagnosis of mixed dementia (both Alzheimer's and vascular) is confirmed.
Non-Medical Therapies and Daily Living Support
Therapies and practical support are essential for maintaining quality of life. An occupational therapist can help adapt the home environment to make daily tasks safer and easier. Other key strategies include:
- Cognitive Stimulation Therapy (CST): Group activities designed to stimulate thinking and memory.
- Physiotherapy: To help with movement, balance, and mobility problems that may arise after a stroke.
- Establishing a Routine: A simple, consistent daily schedule can reduce confusion and anxiety.
- Communication Aids: Using large calendars, whiteboards, and reminder notes can help with memory and orientation.
In addition to these therapies, some families explore complementary wellness products to help manage symptoms like anxiety or restlessness. For those interested in this approach, you can discover CBD Health Collection.
Lifestyle Changes for Brain Health
Adopting a heart-healthy lifestyle is a critical part of managing the condition. Protecting the heart also helps protect the brain from further damage. Key recommendations include:
- A Balanced Diet: Following a Mediterranean-style diet, rich in vegetables, fish, and healthy fats.
- Regular Physical Activity: Gentle exercise like walking or swimming, as approved by a doctor.
- Stopping Smoking: Smoking significantly damages blood vessels.
- Limiting Alcohol: Reducing alcohol intake helps manage blood pressure.
- Staying Active: Engaging in social activities and hobbies to support mental wellbeing.
Finding the right combination of medical, therapeutic, and lifestyle support is key. For help locating specialised dementia care services in your area, you can find the care you need on our platform.
Planning for Future Care: From Home Support to Care Homes
As dementia progresses, the level of support a person requires will change. Planning for future care needs is essential. This allows you to make considered decisions and arrange financial and legal matters, such as a Lasting Power of Attorney, in advance. The step-by-step nature of conditions like vascular dementia means that needs can shift, making early planning a practical necessity.
This long-term planning naturally extends to end-of-life preparations. While it is a difficult subject, understanding the options in advance can relieve future stress for the family. For instance, families may begin to research local services, and looking at examples of support from different providers, such as funeral homes Sydney, can help clarify the process.
Understanding the available care options in the UK helps you to match the right support to the specific stage of the condition.
Care at Home (Domiciliary Care)
In the early to moderate stages of dementia, domiciliary care can be an effective solution. A professional carer visits the person's home to provide support. This allows your loved one to remain in a familiar and comfortable environment for longer. Services can be tailored to specific needs, including:
- Assistance with daily tasks like cooking and cleaning.
- Personal care, such as help with washing and dressing.
- Companionship and support to attend appointments.
- Ensuring medication is taken correctly and on time.
Residential and Nursing Care Homes
Considering a care home is often necessary when a person's needs become too complex to be met safely at home. This may be due to safety concerns, such as wandering or falls, or because the strain on family carers has become unsustainable. It is important to understand the difference between care home types.
- Residential Care: Provides 24-hour personal care, support, and accommodation. It is suitable for individuals who can no longer live independently but do not have significant medical needs.
- Nursing Care: Offers the same support as a residential home but also has qualified nurses on-site to manage complex medical conditions, which can be a factor in vascular dementia.
When choosing a home, look for providers with specialist dementia units or staff who have received specific training. In England, the Care Quality Commission (CQC) inspects and rates all care providers. Always check the latest CQC report to assess the quality and safety of a service.
Finding the right long-term care is a significant decision. Use our directory to find specialist dementia care homes near you.
Your Next Steps in Managing Vascular Dementia
Understanding the journey of vascular dementia begins with recognising its symptoms and securing a clear diagnosis. While a cure is not yet available, a combination of medical treatments and strong support strategies can make a significant difference to quality of life. Proactive planning for future care is a vital step in ensuring your loved one receives the appropriate support as their needs evolve.
When the time comes to arrange professional support, navigating your options is crucial. Our comprehensive UK directory is designed to simplify this process. We provide detailed listings of CQC-rated care providers, clear guidance on funding, and a complete directory of home care, residential, and nursing homes to help you make an informed decision.
Take control of your search and find the right support for your family. Find The Care You Need using our comprehensive UK directory and move forward with clarity and confidence.
Frequently Asked Questions
What is the life expectancy for someone with vascular dementia?
Life expectancy varies significantly between individuals and depends on several factors. These include the person's age, overall health, and the severity of the damage to the brain. While the average is around five years after symptoms begin, many people live much longer. Consistent medical care and management of underlying cardiovascular conditions, such as high blood pressure, can have a positive impact on prognosis. A GP or specialist can provide a more personalised outlook.
Can vascular dementia be prevented or reversed?
Brain damage from a stroke or poor blood flow cannot be reversed. However, you can take steps to reduce the risk of developing vascular dementia or slow its progression. Managing cardiovascular risk factors is key. This includes controlling high blood pressure and cholesterol, maintaining a healthy weight, not smoking, limiting alcohol intake, and staying physically active. Regular health check-ups with a GP can help monitor and manage these risks effectively.
Is vascular dementia hereditary?
Most cases of vascular dementia are not directly inherited. The condition is primarily linked to the health of your blood vessels and cardiovascular system. However, some risk factors that contribute to it, such as high blood pressure or diabetes, can run in families. Additionally, very rare inherited conditions can cause vascular dementia, but this is not typical. The focus for most people should be on managing lifestyle and cardiovascular health rather than genetic predisposition.
How do you communicate effectively with someone who has vascular dementia?
Clear and patient communication is essential. Speak slowly and use simple, short sentences. Make eye contact and ensure you have the person's attention before you begin talking. Minimise distractions like a loud television. Ask simple, closed questions that require a yes or no answer. Be patient and allow plenty of time for them to respond. If they struggle to find a word, offer gentle suggestions. A calm and reassuring tone is always helpful.
What financial support is available for dementia care in the UK?
Several forms of financial support exist in the UK. Depending on circumstances, a person with dementia may be eligible for Attendance Allowance (if over State Pension age) or Personal Independence Payment (PIP) (if under State Pension age). You may also qualify for a Council Tax reduction or discount. The first step is to contact your local council to request a free care needs assessment, which determines the level of support required and potential funding eligibility.
Does the personality change with vascular dementia?
Yes, personality and mood changes are common with vascular dementia. This occurs because the condition damages parts of the brain that regulate behaviour, emotion, and judgement. You may notice changes such as apathy, depression, anxiety, or increased irritability and agitation. In some cases, a person may seem to lose their social inhibitions. Understanding that these changes are caused by the disease, not the person, is an important part of providing care.